What an amazing experience it was.
Right Internal Jugular
An angiogram, which is an X-ray test using a special dye and camera to take pictures of the blood flow in the vein, was performed in the right internal jugular vein. This revealed a short segment stenosis adjacent to the confluence of the brachiocephalic vein. The diameter reduction associated with this stenosis was approximately 60%. The more important number, relative to flow restriction, is the cross sectional area reduction which in this case was approximately 85%.
Multiple collateral veins were noted at this location. Collateral veins indicate attempts by the body to establish bypass flow around an obstruction. Dr. Sclafani inserted the intravascular ultrasound device (IVUS) and confirmed the stenosis. A balloon was inserted, and the vein was dilated multiple times. Another angiogram was performed after dilation which indicated improved flow, diminished flow through collaterals, and no stenosis. Note that the nominal diameter of this blood vessel was 12 mm. Dr. Sclafani prefers to slightly over-dilate the vessel in these instances, and so a 14mm x 4 cm balloon was used. Click on any image to enlarge it.



From left to right, the first image shows the stenosis during angiogram. The second image shows the balloon partially inflated. Note evidence of the stenosis resisting dilation. The third image shows the vein fully dilated.
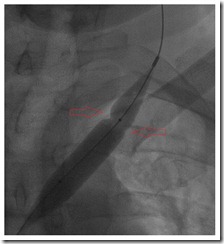
Left Internal Jugular
An angiogram was performed in the left internal jugular vein. This revealed a stenosis at the confluence with the subclavian vein. The degree of narrowing was similar to that in the right internal jugular vein, approximately 60% diameter reduction and 85% cross sectional area reduction. Collateral veins were noted at this location. The IVUS probe was inserted and confirmed stenosis. A 14 mm x 4 cm balloon was inserted, and the vein was dilated multiple times. Another angiogram was performed after dilation which indicated improved flow, diminished flow through collaterals, and no stenosis.

The above image shows the stenosis during angiogram.

The above images show the balloon during inflation. Note evidence of the stenosis resisting dilation.

Above, angiogram after dilation, showing improved flow through the vein.
Azygos Vein
An angiogram was performed and indicated an abrupt lack of filling approximately 4 cm from the junction between the azygos and the superior vena cava. Dr. Sclafani inserted the IVUS device, which revealed a valve that was failing to completely open. This area was dilated with a 10 mm x 2 cm balloon. Note that the nominal vessel diameter at this location was approximately 8 mm. Another angiogram was performed, and improved flow was noted.
Above is an image of a shorter balloon being used to dilate the azygos at a relatively sharp turn in the vein.
Vertebral Veins
An angiogram was performed on the right vertebral vein. Stenosis was noted, but not treated. This is a smaller vein, and Dr. Sclafani was not comfortable performing angioplasty on it.
An angiogram was performed on the left vertebral vein, indicating that the vein branched into two smaller veins, which is abnormal. No treatment was attempted.
IVUS Images
Dr. Sclafani is innovating the use of IVUS technology in CCSVI diagnosis. I’ll have to take Dr. Sclafani’s word regarding what these images show. Maybe they are like the 3-D pictures that were so popular in the 1990’s. You remember- stare at them long enough and you see dolphins jumping over rainbows (or am I thinking about something else altogether). Anyway, here are some example images.


Above, the image to the left shows narrowing of the left internal jugular vein. The image to the right shows the same vein distended during inspiration (breathing in). Wait! I think I see it now. Do you?


The images above show an incompletely opening valve. I kinda see it.
Significance of findings and treatment
Most of the public discourse regarding CCSVI has been regarding the internal jugular veins and the azygos vein, so I will address these first. All three veins showed some type of stenosis, which is a significant finding. The fact that all three stenoses were repaired after angioplasty is potentially significant for my disease progression.
On the other side of the equation, it is unknown whether the repair of these stenoses will be permanent. Furthermore, since most of my lesion load is in the cervical spine, it is unclear how much benefit I will see from even permanent treatment of stenoses in the internal jugular veins.
The findings of stenosis in the vertebral veins may be significant, given the location of my primary lesion load. In my situation, the vertebral veins may be a more important factor than they are in patients with a lesion load primarily in the brain. This remains to be seen.
Below is an MRI image of my cervical spine. This is the problem we are trying to solve (or at least halt the further progression of). Arrows indicate MS lesions.
The Bottom Line
I had abnormalities in five out of five veins examined- all are blood vessels that drain my central nervous system. Therefore, it can be said that I had significant CCSVI. The three larger veins were all treated with angioplasty. The two smaller vertebral veins were not treated. One day I hope that we can attempt to treat at least one of these vertebral veins.
Only time will tell if Dr. Sclafani’s efforts were enough to slow or even stop the progression of my MS. I can only hope.












